It's Topic Tuesday!
- Purab Kothari
- Feb 4, 2025
- 2 min read
Happy Tuesday, everyone! If you did not know, February is American Heart Month, so let's kick it off talking about Aortic Stenosis and Aortic Regurgitation.
These are both conditions involving the aortic valve, the 4th and final valve your blood encounters in its journey through the heart. Like with any valve, its key role is to selectively allow forward flow when desired, and to stop any flow when necessary. During the cardiac cycle, blood should flow forwards freely during systole (the contracting phase) and should not be allowed to flow backwards during diastole (the relaxing phase). This ensures efficient movement of blood through the heart and to the rest of the body.
Aortic stenosis occurs when the opening of the valve is too small. Often times, this is due to the building up of calcium deposits (calcification) of the valve leaflets that occurs with age. The leaflets become rigid and cannot fully open, restricting blood flow. This process is similar to mineral deposition in water pipes, increasing resistance through the pipes.
In response to this increased resistance, the heart must exert more pressure to pump blood through the narrowed valve. Over time, this extra workload can lead to hypertrophy, where the heart muscle thickens. While this initially compensates for the stenosis, this thickening can eventually compromise the heart's ability to pump efficiently, leading to symptoms like chest pain, fatigue, shortness of breath, and even fainting.
Other common causes of aortic stenosis include congenital bicuspid aortic valve (where the valve has two leaflets instead of three), and rheumatic heart disease. Bicuspid aortic valves are more likely to become calcified over time, and rheumatic heart disease can cause scarring of the valve.
Aortic regurgitation (or aortic insufficiency) occurs when the aortic valve fails to close completely, allowing blood to flow backward into the left ventricle after it has been pumped out. This backwards flow overfills the heart, which must now accommodate both the returning blood and the new blood entering from the left atrium.
Over time, the heart responds by dilating, reducing its efficiency and eventually leading to symptoms of heart failure. This can manifest as fatigue, shortness of breath, palpitations, and swelling in the ankles and feet due to fluid retention.
Causes of aortic regurgitation include congenital valve defects, endocarditis (infection of the heart valve), rheumatic heart disease, and complications from aortic dissections or aneurysms, where the structural integrity of the valve or surrounding aortic tissue is compromised.
So how do you treat aortic stenosis and regurgitation?
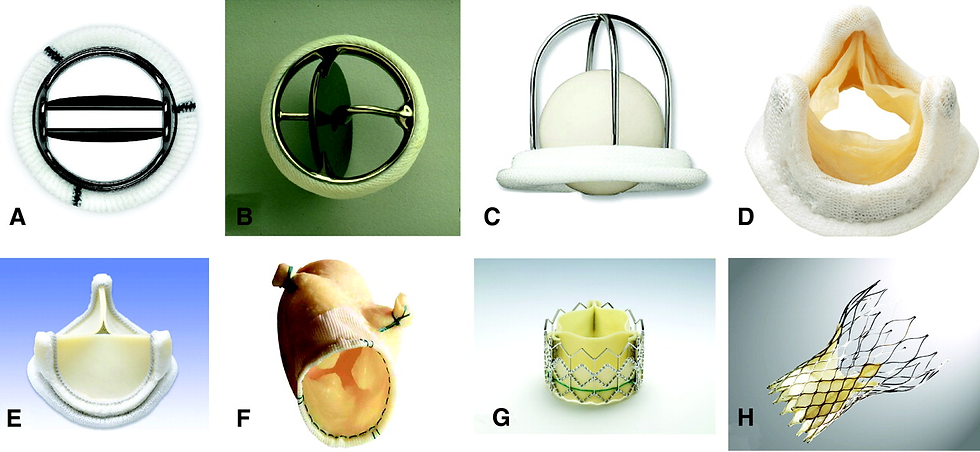
Mild cases of both stenosis and regurgitation are followed with careful monitoring and don't require any intervention. Once severe enough, aortic stenosis may require surgical or catheter-based treatment. Aortic Valve Replacement (AVR) can be performed both surgically or via catheter. Alternatively, your physician may recommend a balloon valvuloplasty, a catheter-based approach where a balloon pushes the valve open. Aortic regurgitation of sufficient severity may also be treated with surgical or transcatheter replacement, or may be treated by Aortic Valve repair (AVr) in select cases to fix the regurgitation while preserving the valve.
That's it for our Topic Tuesday! Be on the lookout for future posts diving deeper into these treatment options. Thanks for joining and I hope to see you next week!
-Purab Kothari





Comments